Liver disease and the diet
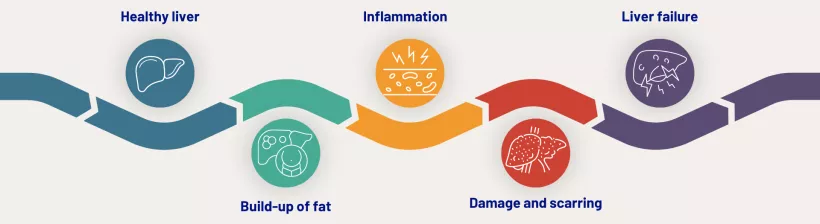
A healthy, balanced diet and lifestyle is important for maintaining a healthy weight and for staying fit and well. If a person exceeds their individual calorie (energy) requirements (i.e., they gain weight), this can increase liver fat content and increase their risk of MASLD (6). Most research looking at excess calories and risk of liver disease has focused on dietary fats and sugars.
Evidence suggests that exceeding calorie requirements, by consuming excess dietary fats or sugars from sugars-sweetened beverages, may increase the risk of MASLD (6). When dietary sugars are consumed as part of a diet where calorie intake is matched to calorie requirements (i.e., calorie neutral/body weight neutral), the effect on liver fat content is less clear, with most studies reporting no significant effect (7).
Fructose and the liver
The effect of fructose-containing sugars on markers of MASLD appears mediated [driven] by both energy control and food source (7)
Fructose, as an added (or free) sugar in the diet, may play a unique role in the development and progression of MASLD, due to the difference in the way it is metabolised in the liver, compared to glucose. However, studies looking at this often use high doses of fructose, with a background diet exceeding a person’s calorie requirements. It is unclear if there is an increased risk of MASLD when consuming fructose-containing foods and drinks as part of a typical calorie-neutral diet. A recent review of the evidence, conducted by researchers at the University of Toronto, concluded that food source (i.e. the type of food), and calorie control, are important factors which influence the effect of fructose-containing sugars on the risk of MASLD (7). The review found that:
- In dietary interventions, when sugars-sweetened beverages (a source of fructose) were consumed at high doses and providing excess calories, there was an increase in liver fat and liver enzymes. Other fructose-containing food sources did not have a significant effect when consumed as extra calories (7).
- When fructose-containing foods and beverages were substituted for other sources of carbohydrates (glucose, sucrose, or starch), with no change in total calories in the diet, there was no independent effect of fructose. This suggests that the effect of fructose is not different from other carbohydrates in the diet (7).
- Further longer-term research is required, using doses of fructose-containing foods and beverages typically found in the diet, consumed at different levels of calorie control (excess and neutral).